A reminder about osteoarthritis
Remember that osteoarthritis is primarily a degenerative disease of the cartilage causing inflammation which is responsible for the pain, unlike other rheumatic diseases that are purely inflammatory (and whose suffix is "itis" as in arthritis). That is why all osteoarthritic impairments of the joints end with the suffix "osis" (such as gonarthrosis).
A joint is the constant contact of two surfaces composed of: cartilage, a joint casing of which the inner layer, called the synovium, produces a fluid that lubricates and nourishes the joint (called synovial fluid), sometimes a meniscus, and ligaments that hold together the two parts of the joint.
Normally, the synovial fluid prevents virtually all friction of the joint surfaces.
In the process of osteoarthritis, the cartilage first changes colour and consistency. It absorbs shocks less effectively, then fissures, erodes, becomes thinner and may even eventually disappear. In disintegrating the deteriorated cartilage may produce an inflammatory reaction of the synovium, thus leading to a painful inflammatory response and excessive secretion of synovial fluid.
When is surgery indicated for osteoarthritis?
There are two aspects: preventive surgery and curative surgery
Preventive surgery
Preventive surgery can restore the correct mechanical conditions in case of anomalies of the joint: congenital hip dislocation, genu valgum, genu varum, scoliosis, etc. that may be responsible later for the formation of osteoarthritis.
Congenital dislocation of the hip
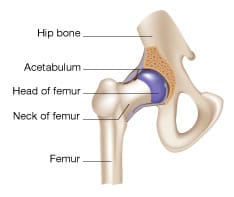
The hip joint consists of the proximal femur (the femoral head) which fits over the pelvis in an osteochondral cavity: the acetabulum.
Real hip dislocation is very rare at birth. What is common is "hip dysplasia" or "subluxation of the hip", that is to say, a hip likely to dislocate on walking if no preventive treatment is undertaken.
Early detection followed by the appropriate treatment will prevent dislocation and replace the femoral head in the acetabulum.
The paediatrician who examines a newborn baby or an infant always systematically looks for the existence of a subluxation of the hip, especially since talks with the parents can enable finding risk factors such as:
- family history of hip dislocation
- predisposing geographical origin (Brittany, Creuse, Auvergne, the Po Valley, etc.)
- breech delivery
- malposition of the feet
- etc.
Ultrasound of the hips is widespread and can be performed at the age of 2 months. It allows you to diagnose subluxation of the hip without irradiating the infant.
The radiological examination is performed to confirm an abnormal ultrasound image at around 4 months.
TreatmentIn newborns with a subluxation of the hip, the treatment needs to be very simple. It is necessary to maintain the legs flexed and thighs apart during the first months of life. The femoral head will thus place itself in the socket which will mould itself around it.
Several techniques are possible in abduction langeage but consultation with an orthopaedic surgeon is needed to make a choice.
In severe cases of late detected hip dislocation, surgical treatment is necessary. Only your doctor can assess the need for such action.

Genu valgum is a deformation of the lower limbs: in a standing position from the front, knees are in contact while the medial malleolus of the ankles are at a distance from one another.
Only very severe cases of genu valgum which persist into adolescence justify surgery. The proposed treatment is then an internal epiphysiodesis (temporary fixation with staples) of the knee (femur or tibia depending on the site of the valgus).
Genu varum is defined clinically by the presence of an intercondylar distance greater than 3 cm, the kneecaps being bowed and the ankles in contact. This anomaly gives a "cowboy" looking silhouette.
You must not worry: genu varum is physiological as children begin walking and it is even more pronounced if the child is heavy and they start walking early. It usually disappears by the age of 18 months to 2 years.
Any genu varum that persists after the age of 2 ½ is pathological. It is then necessary make a radiographic assessment of both limbs to find the cause.
One of the surgical causes to look for is Blount's disease. This is an abnormality of the medial tibial plateau which is visible radiologically.
In this case the treatment is often surgery if the genu varum is severe.
Scoliosis is a deformity of the vertebral column causing a twisting of the spine (backbone) and deformity of the thorax, abdomen and paravertebral areas (near the spine).
It is most often idiopathic (no cause found), but it can complicate disabling disorders (neurological and neuromuscular disorders) and risks to exacerbate the disability.
Whether the deformation is congenital or acquired, whether or not there is muscle weakness, correction can be obtained by intensive corrective exercises and by the appropriate sports such as swimming, wearing a corset or rectifier support, or one or more surgical procedures.
Do not expect physiotherapy to make scoliosis curvature disappear completely, however, it is an indispensable adjuvant treatment of scoliosis irrespective of other treatments used (postural rehabilitation, body in corset, stretching, etc.).
Curative surgery

Curative surgery (osteotomy, muscle sections) may be useful in certain cases of osteoarthritis of the hip and knee.
For the knee, there are different possibilities of prostheses.
- The unicompartmental prosthesis between femur and tibia. It can replace the surface of the knee when only one side of the knee (internal or external) is damaged by osteoarthritis. It has many advantages, but as with any surgery, it requires strict selection criteria. It is therefore advisable to contact a surgeon specialising in the fitting of prostheses.
- The sliding total knee prosthesis. This is the most common prosthesis and it can be placed on any knee.
- The hinged total knee prosthesis. It is the pioneer of prostheses and is no longer used except in very specific situations.
- Prosthesis between the femur and patella. It is uniquely indicated in the isolated osteoarthritis of this knee compartment. This wear is certainly very common, but is generally well tolerated because it is not the weight-bearing area of the knee. The pain is permanent and easily aggravated by the stress on the patella (stairs, squatting or kneeling work), but only exceptionally so bad as to justify an operation. This is why this prosthesis is one of the less common as osteoarthritis of the patella is the most frequent.
This is not a prosthesis. It is an operation indicated when osteoarthritis affects one side of the knee, either outside (genu varum) or inside (genu valgum). The cartilage on the other side being in good condition, the osteotomy will correct the axis of the leg to carry the body weight on the healthy side.
This procedure involves cutting and removing a corner of the tibia, just below the knee, either outside (genu varum) or inside (genu valgum), and fastening the two ends with a plate and screws to restore the "normal" axis of the knee.
The main advantage of this technique is that you keep your original knee: later on a prosthesis will be just as easy to fit as on a knee operated on for the first time. So this is the preferred solution for patients under 60 years of age. It is, however, less recommended after the age of 60 years or for patients in a poor state of health due to the prolonged immobilisation it involves.