The image of osteoarthritis is readily associated with that of old age. It is often seen as an almost natural consequence of ageing. However, this is incorrect because while age is a risk factor for osteoarthritis it is not sufficient in itself to induce the disease.
The frequency of osteoarthritis among young people is lower than in the elderly, but in certain circumstances osteoarthritis can affect young people.
I have bowed legs. Do I risk getting osteoarthritis of the knees?
genu varum
Deformation of the axis of the leg may be a factor for osteoarthritis.
You can have "genu varum" with both knees that deviate from one another :
it is a fairly common morphology. The displacement of the centre of gravity inside the knee increases the internal pressure in the cartilage of the joint between the femur and the tibia and can therefore promote the occurrence of osteoarthritis at this site.

genu valgum
Conversely, "genu valgum" is the cause of knees that are closer to one another while the ankles are further apart. But saying that "genu varum" is a predisposing factor does not mean that you will definitely suffer from osteoarthritis of the knee. The combination of clinical signs (pain, stiffness, deformation) and X-rays will help your doctor make the diagnosis of osteoarthritis and especially to consider a preventive treatment.
A surgical procedure is not necessary if you are not experiencing any pain.
I am a young 24 year old woman and I am a little "too curvy".
Do I risk getting osteoarthritis?

There is a definite correlation between being overweight and osteoarthritis of the knee or hip. Excess weight plays a mechanical role, but it is not the only cause since, according to some studies, being overweight also influences osteoarthritis of the hand. Other studies also show that subjects with osteoarthritis of the knee at the age of 40 will see their osteoarthritis develop more slowly if they can permanently lose weight.
It is important that you carry out a dietary assessment with your doctor and then follow a diet to prevent or delay the onset of disabling pain and stiffness. Of course, fighting against obesity will also enable you to considerably reduce this significant risk factor with regard to cardiovascular diseases.
My parents told me that as a baby I had a congenital dislocation of the hip.
Do I risk getting osteoarthritis of the hip?
There may be trigger factors, if not aggravating factors.
Some diseases of the hip, congenital or developmental, can lead to osteoarthritis later in life. The 2 main anomalies of development are:
- coxa vara also known as adolescent coxa vara
- congenital dislocation of the hip
First of all, some basics of anatomy: the coxa vara is an abnormal decrease in the angle between the femoral head and femoral shaft. This deformity occurs in most cases at the time of the rapid spurt of growth in adolescence.
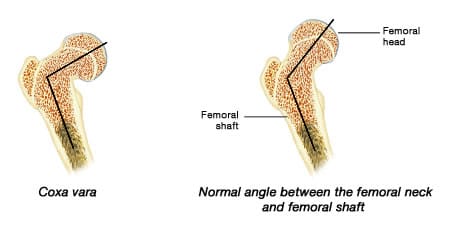
In normal adults, the angle between the neck and femoral shaft is 120 degrees to 135 degrees. If the angle is reduced to less than 120 degrees, it is a coxa vara.
In the event of coxa vara, there are two possibilities for surgical treatment:
- osteotomy which consists in straightening the axis of the leg to balance the functioning of the hip. This is the real treatment of the cause.
- total hip replacement which is intended to replace the worn cartilage, but is used only if the cartilage has been destroyed (at an advanced stage).
Formerly, dislocation of the hip was a misdiagnosed condition. And it led to a large number of cases of osteoarthritis of the hip.
Nowadays hip dislocation is systematically sought from birth and during the first consultations of newborn babies. Once the diagnosis has been made, it is usually sufficient to change the baby in abduction (legs spread apart) to permanently reduce the dislocation.
I am a young sports person and the cruciate ligament in my knee has ruptured.
I have been told that I risk getting osteoarthritis of the knee. Is this really true?
Knee osteoarthritis is a degenerative lesion "gradually becoming established" over the years. The violent trauma which involved the region of your knee joint resulted in a forced and abnormal movement of the joint. As your skeleton resisted the trauma as a result of the surfaces of the two bones temporarily moving apart, the ligament was stretched or torn.
Consequently, one can observe 2 levels of ligament injuries:
- a slight sprain due to simple ligament stretching, with minor tears, which does not involve abnormal movements of the joint.
- a serious sprain due to a torn ligament which may extend to total rupture of one or more ligaments. This will lead to abnormal joint movement causing instability of the limb which is what will be looked for during the physical examination.
If necessary, particularly in cases of instability in the joint of your knee, your doctor will suggest early stabilisation type surgery. In the past, certain surgical procedures could lead to osteoarthritis. Nowadays these techniques have been abandoned and knee surgery presents fewer osteoarthritic complications.

Diagram of the ligaments of the knee joint
The anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL) are inside the joint
The medial collateral ligament or MCL and lateral collateral ligament or LCL are outside of the joint
During an X-ray, radiographic evidence of osteoarthritis was found.
I do not suffer at all but I wonder if I am likely to suffer?
The 3 classic radiological signs evoking osteoarthritis are:
- narrowing of the joint space between bones,
- signs of bone condensation (osteosclerosis)
- bony spurs called osteophytes deforming the edges.
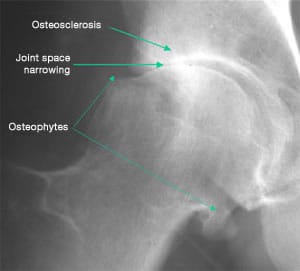
Radiological signs of osteoarthritis
The existence of these signs is evidence of an erosion of the cartilage of the joints involved. However, there is no parallel between the radiological signs and the clinical signs such as pain and joint stiffness. Discovering signs of osteoarthritis is common on X-rays. In most cases, you never suffer from this "osteoarthritis".
Sometimes the clinical signs "speak for themselves" while the radiological damage is "silent" and sometimes, as in your case, the opposite.
In general, these are the clinical signs that guide the treatment. But with your doctor and depending on your case it may already be useful to undergo therapeutic care which can include:
- Fighting against risk factors (excess weight, resting or improving the ergonomics of the joints involved).
- In the event of the onset of pain associated with radiological signs, a treatment may be considered (analgesics, anti-inflammatory drugs, anti-arthritic drugs, etc.).